Hey, Spirit of Autism family! I appreciate your patience regarding the fact that I’ve not been able to keep the Blog up to date while finishing Advanced EMT school. It’s been quite a ride but I’m nearly there! I can see a light (or is it flashing lights?) at the end of the tunnel…
Hey, Spirit of Autism family! I appreciate your patience regarding the fact that I’ve not been able to keep the Blog up to date while finishing Advanced EMT school. It’s been quite a ride but I’m nearly there! I can see a light (or is it flashing lights?) at the end of the tunnel…
I’m going to be transitioning the Blog to focus more on Autism Training Tips for Emergency Responders, Autism Safety Tips (for families and responders alike) and Emergency Preparedness for Autism Households. Previously the focus was on parents and caregivers only, which made it very confusing for those landing on my website, seeing that I do training for emergency responders, but solely reading about my journey as a parent. I will still be sharing lots of stories and personal experiences and of course adding my experiences and perspective as a parent – how could I not? My main focus, however, is to get critical information into the hands of emergency responders that have not yet taken my training course. To do this, I need to start offering it here.
If you have friends and family members in public safety, healthcare security, disaster response, or similar fields, please point them to the website! I want to go beyond local training efforts and start making a global difference.
So, the first in the Weekly Autism Tips for Emergency Responders [W.A.T.E.R.] series is… (sound the horns)…
Sensory Meltdown Vs. Tantrum
When I introduce my course objectives to class recipients, I talk about the definition of Autism, starting with what Autism is NOT. It is not a mental illness and it is not a behavior issue. At this point, students typically turn their heads and look at each other questioningly, as if I’m speaking Swahili. If I had a nickel for every time my son’s inability to cope with an overwhelming sensory environment was labeled a temper tantrum or behavior disorder. And I’m not just talking bystanders, this has happened with Special Ed teachers and pediatric neurologists.
I am a single mom. I’m not going to sit here and tell you that my child has never had a tantrum or behavioral outburst. He’s a BOY. With lots of ENERGY. Going through PUBERTY. Of course there have been times he’s tested those in authority. That’s what teenagers do.
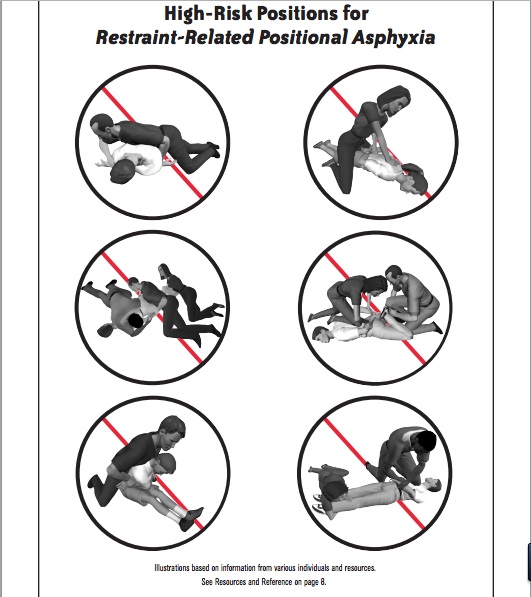
Even knowing all I do about Sensory Processing issues, it is still a fine line to walk when discerning a sensory meltdown and an actual tantrum. I want to help arm you with some real, tangible signs and symptoms to help you tell the difference. Recognizing the physiological differences may change your response and radically alter the outcome of a situation. I’m not ever going to tell you to go against your local protocol or training and put yourself in danger. I’m talking about some really good scene size-up tools to help you respond in the safest way possible for all parties.
Signs and Symptoms of both a Tantrum and Meltdown
If you are just looking at the surface, it is challenging to tell what’s going on – the signs of both tantrums and meltdowns may present as screaming, kicking, shouting, stomping, swearing, biting, throwing, or hitting (either others or self-injurious behavior). Let’s go a little deeper:
A Tantrum typically occurs when a person wants something
A Meltdown is a response to environmental sensory overload or feeling extremely overwhelmed
During a Tantrum the person frequently checks to make sure you are paying attention to their behavior
During a Meltdown the person does not care if anyone is paying attention, they cannot stop themselves
A person acts this way in front of an audience during a Tantrum (behavior will cease when no one is looking)
During a Meltdown the behavior will continue with or without an audience
A Tantrum will cease abruptly once the person gets what they want
In a Meltdown situation, there is no goal – the behavior will cease only when the person can self-calm or when someone helps them regain control
In a Tantrum, there are no residual autonomic nervous system signs following the behavior; the person returns to normal activity within 5 minutes
A Meltdown will yield residual symptoms such as red ears, sweating, and dialated pupils; it takes 45-60 minutes for a person to return to normal following a sensory meltdown
Remember that someone experiencing a sensory meltdown is in survival mode – they are battling their environment and it is pure physical and psychological torture. Their senses are on fire and they have little control over themselves. No one chooses to be in a meltdown, and when you understand what’s happening to the nervous system and help someone through it your are not “giving in to” or “reinforcing” negative behavior. You are throwing someone a LIFELINE.
Stay tuned for future tips to learn more about Sensory Meltdowns and how you can most safely intervene.