Picture this: you respond to a call for a 26 y/o male “not acting right” (that’s about the extent of information WE get from dispatch, anyway
Picture this: you respond to a call for a 26 y/o male “not acting right” (that’s about the extent of information WE get from dispatch, anyway ![]() ). You arrive on scene and are immediately approached by a 5’9” 230-lb male who won’t make eye contact or respond to his name. He proceeds to get too close, won’t slow down or stop on your command, and maybe even reaches out and tries to touch your arm.
). You arrive on scene and are immediately approached by a 5’9” 230-lb male who won’t make eye contact or respond to his name. He proceeds to get too close, won’t slow down or stop on your command, and maybe even reaches out and tries to touch your arm.
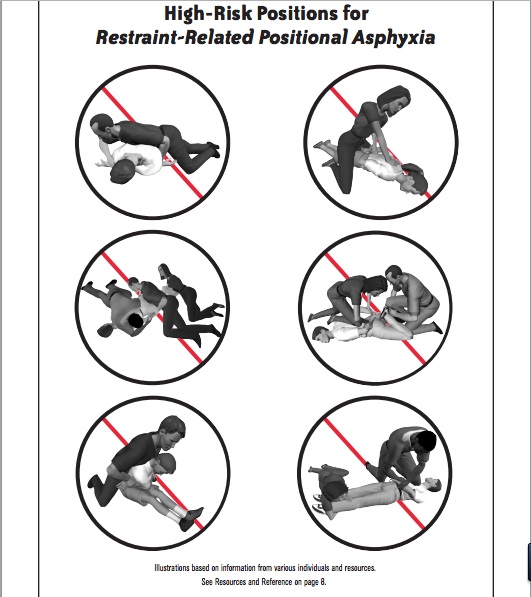
As an EMS provider or law enforcement officer, this situation would immediately be perceived as an aggressive threat and could go south very fast.
Regarding body proximity, responders are often faced with the reactionary gap – the human factors formula that compares action vs. reaction – when assessing situations like this on scene. The closer an assailant is to you, the less time you have to defensively react to any aggressive behaviors or actions.
When an emergency responder experiences a threat, it takes on average .58 seconds to assess and determine if the threat is real, then an additional .56 to 1.0 seconds to make a response decision. We as providers have to fall upon one of five possible responses to threat: defend, disengage, posture, hyper-vigilance or submission. I’m sure you can figure out which one most public safety professionals embrace.
So what if the person was autistic? What if they didn’t understand where their body ends and space begins? What if body proximity, spatial awareness and proprioceptive dysfunction came into play and they had no malicious intent and no idea their actions were perceived as threatening?
Does that mean you should leave yourself unprotected or allow these behaviors on scene? Of course not. But let me explain.
There are four main categories of proxemics:
- Intimate Distance (touching to 2 ft)
- Personal Distance (2-4 ft)
- Social Distance (4-12 ft)
- Public Distance (>12 ft)
Although seemingly effortless to most people, judging the right distance to stand from someone is a complex and dynamic skill. It can depend on many factors, such as your relationship to the other person, your age, gender, emotions, and culture. Your body proximity is a form of nonverbal communication that, in turn, says a lot to another person. Standing too close to someone can absolutely communicate aggression.
Why This Is an Issue
The Autism Genetic Resource Exchange (AGRE) compared the scores of 766 children with autism against 766 of their unaffected brothers and sisters on a questionnaire of autistic social behaviors. An overwhelming 79 percent of autistic children “were less aware of being too close and more prone to personal space invasions” than their neurotypical siblings. Though it seemed to improve with age, it continued to affect teenagers and young adults. Those with spatial issues were more likely to:
- Stand too close to others
- Touch others in an unusual or inappropriate way
- Walk in between two people who are talking
- Be unaware they are talking too loudly or making too much noise
This behavior is often done on automatic pilot and not self-monitored.
Proprioception and Spatial Awareness
Proprioception refers to the sensory input and feedback that tells us about movement and body position. “Receptors” are located within our muscles, joints, ligaments, tendons, and connective tissues.
If this proprioceptive sense is not receiving or interpreting input correctly it is referred to as PROPRIOCEPTIVE DYSFUNCTION.
Spatial awareness is part of our overall perception. Since perception is the organization and interpretation of sensory stimuli from our environment, autistic people would need to have adequate body awareness to be able to form the relationship of their body with the stimuli and objects within that space.
My son has tremendous struggles when it comes to this. Not only does he have to constantly touch the wall when walking in public, he perpetually “hovers,” stands too close to people, touches them without invitation, and even crashes into them. This is due to his nervous system craving proprioceptive input and his inability to fully perceive where he is in relationship to his surroundings. At home, we use a hula-hoop to continually demonstrate personal space. While he has made significant progress, it is something we must address daily.
What scares me is that my son is a BIG child. His simple lack of spatial awareness might cause him to be severely injured or incapacitated if his behaviors are misinterpreted, especially during a heated situation or crisis.
What Can You Do On Scene?
If you identify someone as autistic on scene, whether by the family’s information or from the tools you learned in my autism training, try to keep this information in the back of your mind during your scene size up. Know there is a possibility of someone being a ‘space invader’ and that it might not be an aggressive or threatening action.
I am not telling you to put your guard down and allow someone into your personal space AT ALL. But awareness goes a long way. When you start putting the picture together that someone might have spatial awareness issues or proprioception dysfunction, try putting your arm out and stating, “Stay at arm’s length.” Use clear, concise phrases that have only one meaning, such as “Stop there” while holding your arm out.
The combination of the visual cue and clear commands could truly go a long way in stopping a situation from being misinterpreted and rapidly escalating out of control.